Provider Pulse – October 2022
 Reminder: VA Request for Services Requires Provider Signature
Reminder: VA Request for Services Requires Provider Signature
Please remember to fill out all required fields on all Request For Services (RFS) forms. A signature from the ordering provider in the provider signature box is required.
RFS forms signed by office staff will no longer be accepted. Any supporting documentation must also be included with the RFS form to support VA clinical review and care coordination.
Veterans Affairs Medical Center staff will process a completed RFS usually within three business days, and the provider will then be notified of the approval/denial. If forms received are incomplete, or lack the proper documentation, they may be sent back to the appropriate offices for completion.
For more information on the RFS forms, view the Request For Services Quick Reference Guide.
 Avoid Claims Denials: Submit NDC Codes on CMS-1500 HCFA Form
Avoid Claims Denials: Submit NDC Codes on CMS-1500 HCFA Form
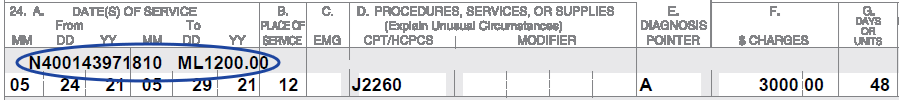
If your practice bills National Drug Codes (NDC) on a CMS-1500 HCFA Form, please submit the NDCs in the shaded portion of Item 24 as 13 position entries (positions 01 through position 13) beginning with the qualifier N4 followed immediately by the 11-digit NDC code (e.g., N499999999999).
It is also a requirement to provide the NDC dosage after the valid NDC number.
Any claims received that do not include the N4 in the correct position will be denied.
Below is an example of how the NDC should be submitted:
 VA Recommends Urine Drug Screens for Veterans Taking Prescribed Opioids
VA Recommends Urine Drug Screens for Veterans Taking Prescribed Opioids
TriWest is working with the Department of Veterans Affairs (VA) to assist providers and promote quality care by helping ensure drug screens are performed on Veteran patients who are prescribed opioid medications.
VA recommends that a urine drug screen be conducted in accordance with the dose and length of treatment for opioid medications, with a minimum screening frequency of twice annually, or every six months.
Urine drug screen testing services are billable services, including those rendered as point of care in the office.
Please review your records to ensure that a urine drug screen has occurred for any Veterans under your care who meet this criteria. If no drug screening has occurred, consider discussing and performing this test with the Veteran(s) at the next appointment, as clinically indicated, as part of a safe and healthy opioid treatment plan.
Training that covers opioid-prescribing practices and recommended safety efforts is provided by VA, and available at www.healthquality.va.gov/guidelines/Pain/cot/.
For a comprehensive review of VA’s training requirements be sure to visit TriWest’s Training Page, which provides access to VA’s Opioid Safety Initiative Training.
 TriWest Introduces New Veteran Appointment Self-Scheduling Program
TriWest Introduces New Veteran Appointment Self-Scheduling Program
A new TriWest pilot initiative launched Oct. 1, 2022, providing Veterans with VA-approved Optometry referrals the ability to self-schedule appointments.
TriWest will initially roll out the new self-scheduling functionality with Optometry referrals only. This is because many Veterans needing Optometry services are already accustomed to scheduling their own eye exam appointments.
Once the Optometry pilot program has successfully been completed, TriWest plans to roll out the Veteran self-scheduling capability to other provider specialties where self-scheduling is advantageous to Veterans.
As with all appointments in the community, Veterans will be required to have an approved VA referral prior to scheduling Optometry appointments with local network providers and facilities of their choice.
For Our Community Care Network Partners: When Veterans Call to Schedule an Appointment
As network providers, TriWest anticipates initially Optometrists, and later other providers, may begin to experience increased Veteran calls regarding scheduling appointments for VA-approved referrals.
Veterans must schedule their appointments within 2-3 days of receiving their initial phone call from TriWest, which may prompt Veterans to call their preferred providers directly prior to reviewing their VA approved referral.
Should network providers receive calls from Veterans, TriWest encourages providers to inform Veterans of the ability to access their referrals for self-scheduling appointments by finding easy instructions under the “Veteran Services” dropdown menu on the TriWest.com home page.
After a Veteran schedules a VA-referred appointment, a provider should remind the Veteran to report back to TriWest within 24 hours, indicating that their appointment has been scheduled. Otherwise, network providers will not receive important details and paperwork from TriWest for the Veteran appointment.
 Provider Handbook Updates
Provider Handbook Updates
There are no updates planned for the CCN Provider Handbook. As a reminder, the CCN Provider Handbook is now available in a web-friendly version online.













