Provider Pulse
July 2020
Welcome to July
Here comes the heat! And we’re not just talking about the weather. As we move into July, TriWest Healthcare Alliance continues expanding Community Care Network (CCN) coverage throughout Region 4. Additionally, the Department of Veterans Affairs (VA) has some new required training for providers on opioid safety, and telehealth went into effect as an official benefit under CCN. Read all about these hot new items, and more, below.
In This Edition:
- TriWest Expanding CCN Coverage in Region 4
- CCN Approved Referrals Now Being Issued
- NEW! VA Requiring Providers to Take Opioid Safety Training
- Telehealth: An Option for Treating Veterans
- Pharmacy App Now Available on Availity
- Reminder: File Electronic Claims for Speedier Payments
- Provider Handbook Updates
TriWest Expanding CCN Coverage in Region 4
TriWest Healthcare Alliance continues to increase the number of areas in which it delivers health care under the new Department of Veterans Affairs (VA) Community Care Network (CCN) in Region 4. CCN is being deployed in a phased approach, and is currently operational in Montana and eastern Colorado. This month coverage will increase to include Texas, Utah, Wyoming, and the remainder of Colorado.
Expansion will continue to the remaining western states through the end of August 2020. The entire CCN Region 4 includes the western U.S. states of Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Texas, Utah, Washington, and Wyoming.
Other Relevant CCN Region 4 Information
- Once fully implemented by late August 2020, CCN will replace the Patient-Centered Community Care (PC3) program as the preferred national network VA uses to refer out care for Veterans in their community.
- Providers must be fully contracted with TriWest to receive new referrals under CCN to care for eligible Veterans. Some providers may have received auto-amendments to their existing PC3 contracts that do not require a signature, while others need to sign an amendment or new CCN contract to continue to receive new referrals to treat Veterans under CCN. It is imperative that providers sign their contract and submit it to TriWest so they can continue to receive new referrals to care for Veterans under CCN.
- Providers with existing PC3 referrals can complete the associated episode of care and claims will be paid even after CCN begins in their market. If they need to extend the PC3 authorization, they must submit a Request for Services (RFS) directly to VA and a new authorization will be issued under CCN.
PC3 information previously contained on the TriWest Provider portal at www.triwest.com/provider is shifting to the TriWest Payer Space on Availity at www.availity.com. Availity is now our providers’ one-stop shop to access CCN training as well as applications, quick reference guides, the Provider Handbook, and news and announcements.
Claims will continue to be sent to WPS Military and Veterans Health (WPS MVH).
CCN Approved Referrals Now Being Issued
As a result of the Community Care Network (CCN) starting up in parts of CCN Region 4, some providers may receive new CCN approved referrals/authorizations even if they are not in the same geographic area of the “live” VA Medical Center (VAMC).
CCN first began in Montana and eastern Colorado, and the remaining states will go live with CCN in Region 4 by the end of August 2020. Here is a schedule of the Region 4 deployment.
PC3 versus CCN Referrals
Once CCN goes live in an area, a VAMC can no longer generate Patient-Centered Community Care (PC3) referrals and must use CCN referrals instead. A site that has gone live with CCN will have access to all of the providers in the VA’s CCN provider directory, nationwide.
As a result, some providers included in the VA CCN provider directory could receive CCN referrals from a VAMC that has gone live, even if they are not in the same geographic area of the “live” VAMC. For example, any Wyoming providers that have a CCN amendment and are active in the VA database could receive a CCN referral from Montana or eastern Colorado.
Additionally, it is possible during this time that a provider could be listed as both a PC3 and a CCN provider. Whether the provider receives a referral under PC3 or CCN depends on when the referring VAMC goes “live” with CCN. The vast majority of community referrals are local, so the likelihood of a community provider receiving a CCN referral will be driven by when their closest VAMC goes live with CCN.
NEW! VA Requiring Providers to Take Opioid Safety Training
They Trained to Serve Us. Now Train to Serve Them.
The Department of Veterans Affairs (VA) now requires each individual provider within a practice or group who has a DEA number and can prescribe controlled medications to Veterans under the VA Community Care Network (CCN) to register for and complete an opioid safety training process. VA also strongly encourages each provider to complete military and Veteran culture training.
The opioid handout and culture training were developed by VA. TriWest Healthcare Alliance is working to inform its network providers under CCN about this new requirement. CCN providers have 180 days from July 1, 2020, to download and review the opioid safety handout by visiting https://train2serve.com.
What Will the Training Cover?
The required opioid safety handout is part of the VA Opioid Safety Initiative, a comprehensive strategy to help reduce reliance on opioid medication and improve effectiveness of pain treatment and safety for Veterans. It consists of downloading and reading a two-page fact sheet.
The recommended military culture training emphasizes the importance of knowing the influence of military culture to improve treatment outcomes for Veterans. According to VA, Veterans who were seen by culturally-informed providers reported they were more satisfied with their visit, and therefore more comfortable seeking and sharing information about their health care needs.
What Happens if Providers Don’t Take the Training?
Each individual TriWest network provider under CCN with a DEA number must download and review the opioid safety handout within 180 days from July 1, 2020. Providers who do not take the VA-mandated training within that timeframe could result in them not receiving new Veteran referrals until they complete the training.
Next Steps – Take the Training!
To register and download VA’s opioid safety requirements:
- Visit https://train2serve.com.
- Select "Register Now."
- Complete the registration process.
- Download the Opioid Safety Initiative information.
TriWest thanks you, our network providers, for supporting the important mission to care for our nation’s Veterans. We value your partnership.
Telehealth: An Option for Treating Veterans
TriWest network providers can utilize virtual or phone visits to treat Veterans and provide continued care while staying in compliance with the Centers for Disease Control and Prevention (CDC) COVID-19 guidelines.
While providers rendering services under a Patient-Centered Community Care (PC3) authorization may temporarily conduct telehealth visits due to the COVID-19 (Coronavirus) pandemic, telehealth is a new benefit under the Community Care Network (CCN) and was not implemented solely due to COVID-19. All telehealth services must comply with state regulations and any additional criteria established by the Department of Veterans Affairs or TriWest. This may include Veteran culture training, platform compatibility, and compliance with billing and medical document timeframes.
Telehealth Billing for COVID-19
Physicians and practitioners who have transitioned to telehealth due to COVID-19 should submit claims with the place of service (POS) code that would have been reported if the service was rendered in person. For example, if you normally see a Veteran in your office, submit claims using POS 11 (office) and modifier 95 to indicate this is telehealth due to COVID-19.
The use of the office POS location ensures appropriate reimbursement for services which would have otherwise occurred in person, but are temporarily provided via telehealth. This is the same rate providers are paid if the services were in person. This is all in alignment with current Medicare policy. Whether Medicare will extend this policy beyond the current COVID-19 pandemic is unknown at this time.
Also, Medicare policy uses POS codes instead of the GT modifier to indicate the place of service. To ensure your claims are NOT seen as standard telehealth claims, but instead telehealth due only to the COVID-19 pandemic, use the correct POS code and do not include the GT modifier.
Using a POS of 02 (telehealth) indicates you are providing a standard (not COVID-19) telehealth service. If you have historically provided telehealth services, you should continue to use the 02 place of service.
If you have filed a claim with the inappropriate POS or modifier code, submit a corrected claim to TriWest’s claims processor WPS Military and Veterans Health (WPS MVH) to have it reprocessed. Providers should put a “7” in the resubmission code field (field 22) on a CMS 1500/837P claim form for corrected claims.
For better understanding of Medicare policy, please take a look at these Medicare frequently asked questions.
General Telehealth Guidelines
Regardless of whether you’re providing telehealth services due to COVID-19, or as a new benefit under CCN, please follow the telehealth guidelines below:
- Providers must have an authorization on file before proceeding with telehealth care.
- The Standardized Episode of Care (SEOC) authorization letter for primary care includes CPT codes to cover virtual treatment.
This guidance currently applies to all specialties including Behavioral Health.
For more information regarding telehealth, TriWest has developed a Telehealth Guidelines Resource Page. There also is a special telehealth section in the CCN Provider Handbook.
Pharmacy App Now Available on Availity
Community Care Network (CCN) urgent care and emergency care network providers can now look up the medication they’ve prescribed to Veterans via the Real-time Pharmacy Application on the TriWest Payer Space on Availity.com.
Providers can search by Member ID or claim number. Once a match is found, the fields will auto-populate with the claim number, Veteran’s name, ID, and group number. It will also show the prescription number, brand, quantity, days’ supply, prescriber, and pharmacy.
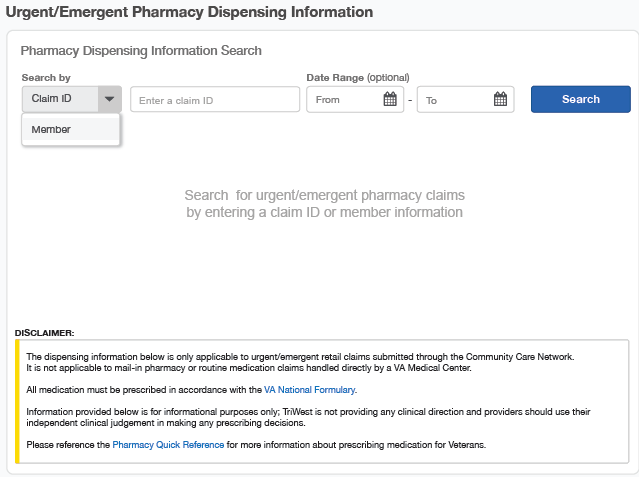
The dispensing information found on the TriWest Payer Space on Availity is only applicable to urgent/emergent retail claims submitted through the CCN. It is not applicable to mail-in pharmacy or routine medication claims handled directly by a Department of Veterans Affairs (VA) Medical Center.
All medication must be prescribed in accordance with the VA National Formulary.
Remember that the information provided on Availity is for informational purposes only. TriWest is not providing any clinical direction, and providers should use their independent clinical judgement in making any prescribing decisions.
Please reference the Pharmacy Quick Reference Guide for more information about prescribing medication for Veterans.
Reminder: File Electronic Claims for Speedier Payments
If you have not already enrolled in the option to submit your claims electronically, do so now by visiting WPS MVH. Filing electronically will speed up your claims processing.
Due to COVID-19, TriWest will be extending Patient-Centered Community Care (PC3) referrals with SEOC end dates of March 1, 2020 – July 31, 2020, to a new expiration of Sept. 30, 2020. TriWest will be updating these authorizations with the new end date. A few SEOC types, such as Inpatient and some Home Health, will be excluded from this update. TriWest apologizes for any claims that were denied prior to the authorization end dates being updated to September 30, 2020.
Providers do not need to revert to paper claims to include the updated authorization paperwork.
Provider Handbook Updates
In August 2020, the following information will be added to the Provider Handbooks:
- CCN Handbook (pages 12-13) and PC3 Handbook (page 11): Based on new information from the Department of Veterans Affairs (VA), community hospitals and providers treating Veterans who self-present to an emergency department should use the following methods to notify VA within 72 hours of Veterans presenting to the emergency room through a new centralized location, the Community Care Centralized Call Center, which is staffed and operated by Office of Community Care (OCC):
- Email: VHAEmergencyNotification@va.gov
- Phone: 844-72HRVHA (844-724-7842)
- CCN Handbook (pages yet to be determined): Providers who have filed a CCN claim to care for Veterans will be encouraged to take a VA quarterly survey about CCN. TriWest highly recommends providers take this survey, as the results will help improve how VA and TriWest administer CCN for providers and Veterans.
- CCN Handbook (pages yet to be determined): Based on new information from VA, TriWest will now be able to pay certain out-of-network providers for services provided under a CCN-approved referral: ancillary providers when services are provided as an adjunct to medical or surgical services provided by in-network providers; and out-of-network facility providers supporting care provided by an in-network physician performing scheduled, non-emergent care.
- CCN Handbook (pages yet to be determined): Section 131 of the Department of Veterans Affairs (VA) MISSION Act of 2018 requires all CCN providers with a DEA number who can prescribe medications for Veterans to complete opioid safety training within 180 days of July 1, 2020. CCN providers who join the TriWest network after July 1, 2020, have 180 days to complete the opioid safety training from the date of their signed and executed contract.













