Provider Pulse – August 2023
 NEW! Submit Claims Reconsideration Forms Electronically
NEW! Submit Claims Reconsideration Forms Electronically
Claims reconsideration forms can now be submitted electronically! The easy online form enables secure and efficient claims reconsideration submissions, and can help save you time without the added tasks of printing and mailing the forms.
This enhancement is part of TriWest’s ongoing commitment to providers, and helps automate and speed up business processes.
Submit a claims reconsideration form when you believe a previously submitted and processed claim was complete and accurate (to your knowledge), but you disagree with the claim determination, and are requesting secondary review.
As a reminder, please submit separate Reconsideration requests for each disputed claim. If you are submitting additional information that was not included in the original claim submission, please do not submit a claim reconsideration request. Any changes to a previously submitted and or processed claim must be submitted via the corrected claims process.
To submit the form electronically, go to the new online Provider Claims Reconsideration Form.
For more on how to file a Claim Reconsideration Form, please review the Billing and Claims section of the Provider Handbook.
 Get Paid Faster with the Availity EFT/ERA Enrollment App
Get Paid Faster with the Availity EFT/ERA Enrollment App
Spend more time caring for our nation’s Veterans and less on claims paperwork and waiting on snail mail with the new Availity EFT/ERA online enrollment tool!
This easy online tool enables secure and efficient EFT/ERA enrollment, and ensures you will save time by receiving automated and direct pay.
Consider the benefits of enrolling in EFT/ERA:
- No enrollment fee.
- No more time-consuming paper checks.
- Receive payments in as little as 10 days.
- Safe and secure funds transfer to your bank account.
To sign up or learn more about the app, visit Availity.com and select My Providers | Enrollment Center | Transaction Enrollment.
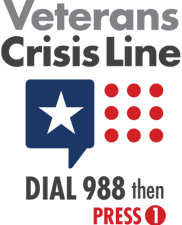
 Emergency Suicide Care Treatment for Veterans: COMPACT Act Update
Emergency Suicide Care Treatment for Veterans: COMPACT Act Update
As a result of the Veterans COMPACT Act of 2020, emergent suicide care for eligible Veterans in acute suicidal crisis at a VA or non-VA facility is a covered benefit. VA has updated COMPACT Act guidelines for acute suicidal crisis care for Veterans.
Veterans meeting certain criteria are eligible for urgent care or emergent care if in an acute suicidal crisis. A trained crisis responder or health care provider must diagnose the Veteran's eligibility, using given criteria, to activate this benefit.
Read more about the COMPACT Act and Veteran coverage for acute suicidal crisis in the CCN Urgent Care & Emergent Care Quick Reference Guide.
 Check Your Referral and Authorization Status Using HSRM
Check Your Referral and Authorization Status Using HSRM
Check each step in the status of your referrals and authorizations by using HealthShare Referral Manager (HSRM).
HSRM is VA’s tool to manage and simplify the entire care coordination process all with less turnaround time. By utilizing HSRM, providers can submit Request for Service (RFS) forms, referrals, authorizations, and other medical documentation, and can expect shorter wait times when contacting the authorizing VAMC regarding Veteran care.
To assist providers and staff, VA is offering online HSRM training through VHA TRAIN.
There should be one point of contact (POC) for each provider/group when filling out an end-user tracker form with information about all staff who are requesting HSRM access.
The POC can email the completed end-user tracker form to the HSRM Community Provider Help Desk at HSRMSupport@va.gov. The Help Desk is also available by phone at 844-293-2272.
 Subscribe to VA’s Provider Advisor Newsletter
Subscribe to VA’s Provider Advisor Newsletter
Get access to the latest Veteran health news when you subscribe to the Provider Advisor, the monthly newsletter from the Department of Veterans Affairs (VA).
If you want to receive more VA health news, subscribe to Provider Advisor.
 Provider Handbook Updates
Provider Handbook Updates
The following content has been added to the Billing and Claims section of the CCN Provider Handbook outlining the new electronic claims reconsideration form.
How to File a Claim Reconsideration
Submit claims reconsiderations electronically by completing the online Provider Claims Reconsideration Form.
The easy online form enables secure and efficient claims reconsideration submissions, eliminating the added tasks of printing and mailing the forms, saving you time and money!
The form can also be submitted by mail. Download and fill out TriWest’s Provider Claims Reconsideration Form, and mail it and all supporting documentation to:
TriWest CCN Claims
P.O. Box 42270
Phoenix, AZ 85080-2270
As a reminder, you must submit separate Reconsideration requests for each disputed item.