Provider Pulse – August 2021
 Help is Available for Afghan Veterans from VA, TriWest
Help is Available for Afghan Veterans from VA, TriWest
Many of the Veterans who receive health care through the U.S. Department of Veterans Affairs (VA) Community Care Network (CCN) have served in Afghanistan. These heroes may be struggling with what they are observing with the ongoing events in Afghanistan and the upcoming 20th anniversary of September 11.
VA and TriWest Healthcare Alliance (TriWest) have not forgotten these Veterans and ask that you, our network providers, take extra care of them at this time. If they need support, please encourage them to reach out to a friend, family member, spiritual leader, or a mental health provider. In addition, there are many VA resources you can direct Veterans to that can be of help to them. A recent newsletter from VA recommends the following resources that you can share with your Veteran patients:
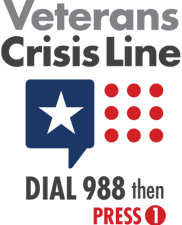
- Veterans Crisis Line - If you are having thoughts of suicide, Dial 988, then PRESS 1 or visit http://www.veteranscrisisline.net/. You can also Chat or Text 838255.
- For emergency mental health care, you can also go directly to your local VA medical center 24/7 regardless of your discharge status or enrollment in other VA health care.
- Vet Centers - Discuss how you feel with other Veterans in these community-based counseling centers. 70% of Vet Center staff are Veterans. Call 1-877-927-8387 or find one near you.
- VA Mental Health Services Guide - This guide will help you sign up and access mental health services.
- MakeTheConnection.net - Information, resources, and Veteran to Veteran videos for challenging life events and experiences with mental health issues.
- Download VA's self-help apps - Tools to help deal with common reactions like, stress, sadness, and anxiety. You can also track your symptoms over time.
- VA Women Veterans Call Center - Call or text 1-855-829-6636 (M-F 8AM - 10PM & SAT 8AM - 6:30PM ET)
- VA Caregiver Support Line - Call 1-855-260-3274 (M-F 8AM - 10PM & SAT 8AM - 5PM ET)
- Center for Minority Veterans
- VAntage Point Blog Series, Let’s talk about Afghanistan: Resources for Veterans and their families
In addition to the VA resources, TriWest has a dedicated PTSD section on its website to help Veterans, providers and the general public help understand PTSD.
Thank you for your continued commitment to meeting the health care needs of our nation’s Veterans and honoring the sacrifices of those we are humbled to serve.
 TriWest to Require Referral Number When Filing CCN, PC3 Claims
TriWest to Require Referral Number When Filing CCN, PC3 Claims
To help improve claims payment accuracy and cleaner claims submissions, TriWest Healthcare Alliance (TriWest) will now require providers to include the Department of Veterans Affairs (VA) referral/authorization number with all VA Community Care Network (CCN) and Patient-Centered Community Care (PC3) claims submissions. If the referral/authorization number is not provided, the claim will be denied. This requirement is effective Oct. 1, 2021.
With PGBA now accepting and processing all CCN claims and any remaining PC3 claims, it is important that you properly submit claims to PGBA with the following documentation, and in the correct format:
- VA referral number AND one of the following:
- 10-digit Electronic Data Interchange Personal Identifier (EDIPI)
- 17-digit Master Veteran Index (MVI) ICN
- Social Security number (SSN)
- Last 4 digits for SSN with preceding 5 zeros i.e., 00000XXXX
It is extremely important that you do not use any extra characters, spaces, or words with the referral/authorization number or the claim will deny. For example, if the referral/authorization number is VA0012345, referral numbers included in the following format would be denied:
- Auth VA0012345
- Auth # VA0012345
- Ref VA0012345
- Ref # VA0012345
- VA 0012345
- VA012345
For more information regarding proper claims submission, please refer to the Claims Submission Quick Reference Guide or the CCN Provider Handbook.
 Don’t Forget to Renew Your Credentials
Don’t Forget to Renew Your Credentials
Every three years, providers must renew their credentials to stay compliant in order to continue to treat Veteran patients. You should receive a reminder to re-credential four months prior to your expiration date, and are given four different reminders to renew.
To re-credential, validate the information on your profile sheet and submit a re-credentialing application sent to you by your point of contact. If you do not re-credential, you will immediately be terminated for being non-compliant and will not be able to care for Veteran patients.
If you have received notice to renew your credentials, please do so as soon as possible. If you miss your deadline to re-credential but still want to treat Veteran patients, you will need to go through the entire credentialing process again.
For questions or concerns, please contact Credentialing@TriWest.com and include in the email your name, tax ID, national provider identifier, and point of contact.
 VA Requires Signature on File for CCN Claims
VA Requires Signature on File for CCN Claims
As a requirement of participation in VA’s CCN, network providers need to have a Signature on File for any Veteran who will receive care. Similar to standard insurance policies, the Signature on File will indicate that the provider is authorized to submit a claim on behalf of the Veteran, and authorizes payment of medical benefits to the provider.
The document, signed by the Veteran and authorizing the provider to submit claims on their behalf, is the only documentation being requested. This is referred to as "Assignment of Benefits." The document must be signed on or before the date of service identified on the request from TriWest. Do not send medical records/notes from the date of service. The only document requested is the Signature on File. Incorrect document submissions will be rejected.
Use the Attachments suite in Availity® to upload your documents with the Signature on File and select the appropriate LOINC T-12058 Signature on File. Find the Attachments suite located under the Claims and Payments section at the top of TriWest’s payer space on Availity. Availity is the multi-payer site TriWest uses to conduct secure transactions with providers.
TriWest to Audit for Signatures
A random sample of providers’ claims will be audited by TriWest each quarter. Providers will receive the audit requests via a notification in Availity (on the portal homepage).
Requests for documents for up to 10 Veterans seen by a provider will be based upon a randomly pulled sample from submitted claims data and based on the number and value of the claims submitted. The forms/documents will be scanned, uploaded, and stored for future reporting in the event they’re requested by VA. Audits will not be conducted on Ancillary Providers.
As a reminder, TriWest leverages Availity as its one-stop shop for all information and training for CCN. You can also access claims status, and find helpful webinars via the TriWest Payer space on Availity. Be sure to update your Availity account to indicate you’re able to send/receive medical documentation.
Have questions regarding the Availity Portal capabilities for TriWest? Visit https://www.availity.com or call Availity with technical issues at 800-282-4548.
 Instances of Slightly Delayed CCN, PC3 Claims
Instances of Slightly Delayed CCN, PC3 Claims
TriWest has successfully transitioned its claims processing to PGBA. TriWest thanks you – our network providers – for your partnership during this claims conversion. Through the process, some CCN and PC3 providers may have experienced a slight delay in claims processing. We ask for your patience during this time and apologize for the delay. Both TriWest and PGBA are working in tandem and have started to process temporarily delayed claims as of Aug. 16, 2021. TriWest and PGBA expect to be current with claims processing within the next four weeks.
If you do not receive payment following the processing, you can obtain claims status from TriWest Claims Customer Service at 877-CCN-TRIW (877-226-8749) from 8 a.m. to 6 p.m. in your time zone or visit Availity to use the secure “Chat with TriWest” feature.
 Provider Handbook Updates
Provider Handbook Updates
CCN Provider Handbook
On Page 17 under Provider Claims Submission, the following language was added:
- Effective Oct. 1, 2021, TriWest requires providers to include the VA referral/authorization number for all claims submission. If the referral number is not provided, the claim will be denied.
- It is extremely important that you do not use any extra characters, spaces, or words with the referral/authorization number or the claim will deny. For example, if the referral/authorization number is VA0012345, referral numbers included in the following format would be denied:
- Auth VA0012345
- Auth # VA0012345
- Ref VA0012345
- Ref # VA0012345
- VA 0012345
- VA012345
On Page 19 under Clean Claims Requirements, the following language was added:
TriWest requires that you include this number on your claim or your claim will be denied.
It is important that you properly submit claims to PGBA with the following documentation, and in the correct format:
- VA referral number AND one of the following:
- 10-digit Electronic Data Interchange Personal Identifier (EDIPI)
- 17-digit Master Veteran Index (MVI) ICN
- Social Security number (SSN)
- Last 4 digits for SSN with preceding 5 zeros i.e., 00000XXXX
It is extremely important that you do not use any extra characters, spaces, or words with the referral number or the claim will deny.
Please include a Type 2 (organization) NPI on all claims. If you are a solo practitioner without an organizational NPI, please use your individual NPI.
Ensure all coding aligns with Medicare criteria, if applicable. When Medicare policy does not apply, please follow language in your authorization information, VA consult notes, the Provider Handbook or other training materials provided by TriWest and VA.
PC3 Provider Handbook
On Page 14 under Submitting Claims, the following language was added:
Effective Oct. 1, 2021, TriWest requires that the VA referral number be included with all claims submission. If the referral number is not provided, the claim will be denied.
On Page 15, the following language was added:
- Include the VA referral number AND one of the following:
- 10-digit Electronic Data Interchange Personal Identifier (EDIPI)
- 17-digit Master Veteran Index (MVI) ICN
- Social Security number (SSN)
- Last 4 digits for SSN with preceding 5 zeros i.e., 00000XXXX
On Page 15, the following language was added:
Clean Claim Requirements
In order for a claim to process and pay, TriWest must have visibility to the appointment in our systems.
Once the provider receives an authorization letter from either TriWest or VA, the referral/authorization number is the unique identifier assigned for each approved referral/authorization’s episode of care. TriWest requires that you include this number on your claim or your claim will be denied.
It is important that you properly submit claims to PGBA with the following documentation, and in the correct format:
- VA referral number AND one of the following:
- 10-digit Electronic Data Interchange Personal Identifier (EDIPI)
- 17-digit Master Veteran Index (MVI) ICN
- Social Security number (SSN)
- Last 4 digits for SSN with preceding 5 zeros i.e., 00000XXXX
It is extremely important that you do not use any extra characters, spaces, or words with the referral number or the claim will deny.
Please include a Type 2 (organization) NPI on all claims. If you are a solo practitioner without an organizational NPI, please use your individual NPI.
Ensure all coding aligns with Medicare criteria, if applicable. When Medicare policy does not apply, please follow language in your authorization information, VA consult notes, the Provider Handbook or other training materials provided by TriWest and VA.
 VA Offering Free Traumatic Brain Injury Training
VA Offering Free Traumatic Brain Injury Training
The Department of Veterans Affairs (VA) will hold a free seminar on Traumatic Brain Injury: Diagnosis and Management on August 26 at 1 p.m. EST. VA CCN physicians, nurses, psychologists, pharmacists, physician assistants and social workers who treat Veterans are invited to attend the webinar.
This training will include information about VA's traumatic brain injury (TBI)/polytrauma system of care, the need to develop an individualized plan of care for Veterans with TBI and how to connect Veteran patients to VA resources. Additionally, participants will learn about online tools and training resources highlighting issues related to Veterans and service members with TBI.
There will be 1 hour of academic credit for AAPA, ACCME, ACCME-NP, ACPE, ANCC, APA, ASWB, JA IPCE, and NYSED SW.
Registration for the course is available on the VHA Train website.
Contact the VHA Train Help Desk via email at VHATRAIN@va.gov for questions/assistance.